Introduction
Ischemic heart disease (IHD) is a prominent contributor to mortality worldwide, with myocardial infarction (MI) representing its most severe manifestation. Pulsed electromagnetic fields (PEMF) treatment shows promise for treating IHD. Nevertheless, the therapeutic impact and underlying mechanism of PEMF in MI are not fully understood.
Objectives
To investigate the efficacy, safety, and mechanisms of PEMF for MI.
Methods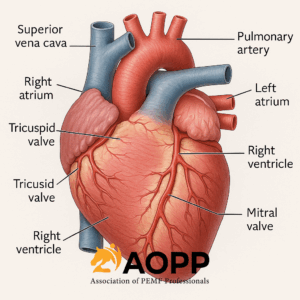
We established MI models in both mice and pigs and performed serial echocardiography and cardiac magnetic resonance follow-up to demonstrate the benefit of PEMF treatment after MI. The pathological environment after myocardial infarction was simulated in vitro to observe changes in various cells exposed to PEMF. Gene knockout (TLR4-/-) mice and inhibitors were used to compare the differences in the efficacy of PEMF treatment relative to that of gene knockout/inhibitor treatments. Agonists were used to further explore the mechanism of PEMF treatment.
Results
In post-MI mice, PEMF treatment enhanced cardiac function and reduced scar formation. PEMF reduced the macrophage inflammatory response, improved cardiomyocyte survival in an inflammatory environment, and decreased collagen secretion by fibroblasts in vitro. Importantly, in the clinically relevant porcine model, PEMF treatment inhibited the inflammatory response and alleviated adverse left ventricular remodeling. Moreover, PEMF could exert therapeutic effects similar to those of gene knockout or inhibitor treatments. In the presence of TLR4 knockout or pyrrolidine dithiocarbamate (an NF-κB inhibitor) administration, PEMF could still improve cardiac function in post-MI mice. Mechanistically, the anti-inflammatory effect of PEMF was reversed when RS09 (a TLR4 agonist) was administered, and the antifibrotic effect of PEMF was attenuated after treatment with SRI-011381 (a TGF-β signaling pathway agonist).
Discussion
In this study, an innovative physical therapy modality was employed in mice and pigs after MI to assess the benefits and safety of PEMF treatment in terms of cardiac anatomical and functional parameters, histopathology, and cellular and molecular responses. Additionally, the mechanisms of PEMF in mitigating inflammation and ameliorating fibrosis were investigated. We demonstrate that i) PEMF treatment can ameliorate cardiac function and reduce scar formation in post-MI mice; ii) PEMF exposure can reduce the macrophage inflammatory response, reduce cardiomyocyte death in an inflammatory environment, and diminish collagen secretion by fibroblasts in vitro; iii) in a clinically relevant porcine model, PEMF treatment has demonstrated the ability to inhibit MI-induced inflammation, reduce cell apoptosis, and alleviate adverse LV remodeling, and the treatment process is safe, with no reported adverse events; and iv) we also revealed that the anti-inflammatory and antifibrotic effects of PEMF treatment are mediated through the TLR4/MyD88/NF-κB and TGF-β1/SMAD3 signaling pathways.
Our study demonstrates that PEMF ameliorates cardiac function in mice following MI, which is consistent with the findings of previous studies [13,14,24]. In addition, many previous studies have shown that EMF can improve oxidative stress by regulating mitochondrial function [25,26]. For example, mitochondriogenesis and respiratory capacity can be enhanced by PEMF exposure [27]. Given the link between oxidative stress and inflammation, these previous findings imply that PEMF has the potential to control inflammation after MI. Notably, our findings in mice indicate that PEMF can alleviate inflammation after MI, which has not been reported in previous MI-related studies. Given the crucial role of timely inflammation control in MI recovery, particularly in the context of irreversible pathological remodeling during advanced stages, our innovative findings provide a key preclinical basis for physical therapy modalities for IHD [28,29]. Moreover, PEMF exposure can reduce the macrophage inflammatory response, decrease cardiomyocyte death, and ameliorate fibrosis in vitro, which further increases our confidence in conducting translational preclinical experiments in large animals.
To achieve clinical translation of PEMF in the treatment of MI, the same efficacy needs to be verified in large animals. Although studies in mice have provided a wider understanding of the treatment of MI with PEMF, the hearts of mice are different from those of humans [30]. In contrast, the pig heart has many similarities with the human heart, both in healthy and MI states [17,31]. There have been many reports on the use of physical therapy modalities, such as low-energy lasers and extracorporeal cardiac shock waves, for the treatment of MI in large animals [32,33]. Of note, there is a dearth of literature pertaining to the impact of PEMF treatment on inflammation and fibrosis in large animals, and our research endeavors to bridge this gap in knowledge. Our study revealed that PEMF treatment modulates systemic and local inflammatory mediators, improves LV function, reduces myocardial scar size, and prevents LV hypertrophy, which is consistent with findings in small animals.
Mechanistically, the anti-inflammatory and antifibrotic effects of PEMF are mediated by two classic signaling pathways, the TLR4/MyD88/NF-κB and TGF-β1/SMAD3 pathways. Multiple lines of evidence support our conclusion: i) The mRNA-seq results of porcine infarct border myocardium suggest that the TLR-like receptor and the TGF-β pathway are critically involved in the therapeutic effects of PEMF; ii) molecular changes in TLR4/MyD88/NF-κB and TGF-β1/SMAD3 were observed at both the cellular and animal levels; iii) The anti-inflammatory effect of PEMF was reversed upon the administration of RS09; and iv) the antifibrotic effect of PEMF was attenuated after the use of SRI-011381.
Inflammation is a key process after MI and is characterized by extensive cell death and inflammatory cell infiltration [34,35]. While an initial surge of inflammation can facilitate the healing process of necrotic myocardium, persistent and elevated levels of inflammation can result in myocardial interstitial remodeling and potentially lead to heart failure [36]. Previous studies have highlighted the therapeutic potential of PEMF treatment for regulating inflammation [37]. Katia Varani et al. have reported significant alterations in both the expression and function of adenosine A2A receptors in human neutrophils treated with PEMF [38]. Furthermore, evidence indicates that PEMF exposure mitigates inflammatory damage in neuron-like cells and microglia [39]. However, the underlying mechanisms and molecular targets of PEMF treatment remain poorly understood. Several in vitro studies reported that magnetic field exposure could reduce inflammatory responses in HEK-Blue™ hTLR4 cells [40,41]. Indeed, the role of TLR4 in inflammation and injury responses, such as those caused by myocardial ischemia, has been demonstrated in many studies using TLR4-/- mice or targeted gene silencing of TLR4 [[42], [43], [44]]. Therefore, in addition to validating the mechanism at the cellular level, we performed a comparative analysis of the efficacy of PEMF and gene knockout/inhibitor in vivo. These results indicate that PEMF can elicit therapeutic effects comparable to those achieved through gene knockout or inhibitor treatment and may have additive benefits when combined with TLR4 knockout or NF-κB inhibitors.
Furthermore, the TGF-β1/SMAD3 signaling pathway plays a crucial role in tissue repair in the early stage of MI, but persistent high expression can lead to the activation of inflammatory factors, angiotensin-II, and other profibrotic cytokines, thereby aggravating cardiac fibrosis [16,45]. The persistent fibrotic response subsequently contributes to cardiac remodeling and the eventual development of heart failure [46,47]. There are currently no studies elucidating the mechanism by which PEMF for fibrosis after MI. The results of mRNA-seq and the trend toward improvement in the WM situation have aroused our interest, illustrating that PEMF may play a role in pathological remodeling. Our study demonstrated that PEMF treatment during MI can efficiently inhibit the TGF-β1/SMAD3 signaling pathway, leading to a reduction in collagen deposition in the border zone of the heart. Both Sirius and Masson staining also revealed a decrease in extracellular collagen. Moreover, the release of TGF-β1 regulates the differentiation of cardiac fibroblasts into myofibroblasts after MI [48]. TGF-β1 is responsible for regulating the transcription of the extracellular matrix gene Col 1 together with the downstream effector SMAD3 [49,50]. We found that the levels of α-SMA (a marker for mature myofibroblasts) and Col 1 were significantly decreased after PEMF exposure in vitro. The underlying mechanism involves the role of the TGF-β1/SMAD3 signaling pathway in the regulation of fibrosis-related proteins.
Importantly, a new treatment should not only have definite efficacy but also safety, which is the key to the clinical translation of treatment. In 2022, the Mayo Clinic commenced a trial aimed at investigating the potential of wearable PEMF equipment to alleviate the burden of myocardial ischemia, which also provides us with the confidence to further explore the clinical efficacy and safety of PEMF [14]. Although the PEMF equipment used in this study is a whole-body intervention, no PEMF-induced adverse events or changes in biochemical parameters were observed. Notably, an increasing number of studies have revealed strong associations between CVDs and the intestinal flora and its metabolites. This connection arises from the fact that metabolites produced by the intestinal flora can elicit an immune response [[51], [52], [53]]. Indeed, the frequency and strength of a magnetic field can influence the growth of the intestinal flora [54]. A previous study revealed that PEMF can induce relevant metabolic adaptations independent of exercise, which is related to their ability to modulate the composition of the intestinal flora [55]. If PEMF treatment leads to the growth of harmful bacteria, it not only affects the efficacy of the PEMF itself but also may cause unnecessary harm to the body [[56], [57], [58]]. Hence, to avoid changes in the intestinal flora during PEMF treatment that might affect the safety of instrument use, we further monitored changes in the intestinal flora of the experimental animals. This also led us to an unexpected discovery of the potential effects of PEMF on intestinal microbial communities in post-MI pigs.
In the present study, we observed that PEMF did not alter intestinal flora diversity in pigs. Nevertheless, PEMF influences the relative abundance of some intestinal flora. Interestingly, these alterations may have positive implications for cardiovascular health. For example, low-density lipoprotein (LDL) cholesterol, a significant risk factor for cardiovascular disease, is positively correlated with Blautia. The relative abundance of Blautia is reduced in the intestines of post-MI pigs following PEMF treatment, implying that PEMF-induced modulation of this bacterium might contribute to improved MI recovery [59]. It has also been reported that the relative abundance of Anaerostipes can increase in individuals with inflammatory diseases, whereas in our study, the relative abundance of Anaerostipes in the intestine of post-MI pigs following PEMF treatment decreased [60]. In addition, Firmicutes and Clostridia have been identified as having a significant correlation with the TLR signaling pathway. The regulation of these microbiotas through fecal microbiota transplantation might downregulate the expression of associated molecules in the TLR signaling pathway, thereby achieving the objective of diminishing inflammation [[61], [62], [63], [64]]. Crucially, correlation analysis in our study also revealed that some intestinal flora with changes in relative abundance were significantly associated with TLR signaling pathway expression. In other words, our findings indicate that the PEMF-regulated intestinal flora may be beneficial for the resolution of inflammation. While this discovery offers a novel perspective, subsequent research is needed to elucidate the precise impacts of PEMF on the intestinal flora and the interconnectedness of this effect with MI.
This study has several limitations. The number of animals used in this study was limited, necessitating further enlargement of the sample size to facilitate clinical translation. Moreover, PEMF-induced cardioprotection may not be explained solely by reducing inflammation and improving remodeling, so other potential mechanisms contributing to the therapeutic effects of PEMF require further investigation. In addition, aminoglycoside antibiotics have been found to attenuate the response to magnetic exposure as well as the potency of the induced secretome [65,66]. The impact of various cellular medium components on PEMF exposure was not evaluated in this study; thus, future in vitro experiments on the magnetic field should place greater emphasis on the design of culture conditions.
Conclusions
In summary, PEMF treatment can ameliorate cardiac function and reduce scar size in post-MI mice and pigs. The benefits of PEMF in the treatment of MI are supported by reduced inflammatory responses, improved cell survival, and decreased collagen secretion. The underlying molecular mechanism of PEMF treatment is associated with the inhibition of the TLR4/MyD88/NF-κB and TGF-β1/SMAD3 signaling pathways. We believe that PEMF treatment holds significant promise as a noninvasive physical therapy modality, justifying further exploration of its potential implications for managing patients with IHD.
